11.3: Health
- Page ID
- 3443
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Objectives
- Describe the nature of health care in the United States.
- Describe and explain some of the special health-care concerns of various segments of American society.
Universal Generalizations
- For Americans the top ten priorities are health care concerns.
- In the United States, Americans spend a higher percentage of its gross domestic product (GDP) on health care than any other nation in the world.
- Managed care has brought down medical costs.
- The inability to get insurance contributes to more serious medical problems among the poor.
- The inability to get insurance contributes to more serious medical problems among the poor.
Guiding Questions
- What are the main issues about health care in the United States?
- What has caused the rapid rise in health care costs in the United States?
- Why are the costs of prescription drugs rising so rapidly?
- What effects has Medicare and Medicaid had on the U.S. society and economy?
- Explain the ways in which poor people suffer disproportionately from healthcare problems.
Health and Theoretical Perspectives
Health refers to the extent of a person’s physical, mental, and social well-being. This definition, taken from the World Health Organization’s treatment of health, emphasizes that health is a complex concept that involves not just the soundness of a person’s body but also the state of a person’s mind and the quality of the social environment in which she or he lives. The quality of the social environment in turn can affect a person’s physical and mental health, underscoring the importance of social factors for these twin aspects of our overall well-being.
Medicine is the social institution that seeks both to prevent, diagnose, and treat illness and to promote health as just defined. Dissatisfaction with the medical establishment has been growing. Part of this dissatisfaction stems from soaring health-care costs and what many perceive as insensitive stinginess by the health insurance industry, as the 2009 battle over health-care reform illustrated. Some of the dissatisfaction also reflects a growing view that the social and even spiritual realms of human existence play a key role in health and illness. This view has fueled renewed interest in alternative medicine. We return later to these many issues for the social institution of medicine.
The Sociological Approach to Health and Medicine
The fact that our social backgrounds affect our health may be difficult for many of us to accept. We all know someone, and often someone we love, who has died from a serious illness or currently suffers from one. There is always a “medical” cause of this person’s illness, and physicians do their best to try to cure it and prevent it from recurring. Sometimes they succeed; sometimes they fail. Whether someone suffers a serious illness is often simply a matter of bad luck or bad genes: we can do everything right and still become ill. In saying that our social backgrounds affect our health, sociologists do not deny any of these possibilities. They simply remind us that our social backgrounds also play an important role (Cockerham, 2009).Cockerham, W. C. (2009). Medical sociology (11th ed.). Upper Saddle River, NJ: Prentice Hall.
A sociological approach also emphasizes that a society’s culture shapes its understanding of health and illness and practice of medicine. In particular, culture shapes a society’s perceptions of what it means to be healthy or ill, the reasons to which it attributes illness, and the ways in which it tries to keep its members healthy and to cure those who are sick (Hahn & Inborn, 2009).Hahn, R. A., & Inborn, M. (Eds.). (2009). Anthropology and public health: Bridging differences in culture and society (2nd ed.). New York, NY: Oxford University Press. Knowing about a society’s culture, then, helps us to understand how it perceives health and healing. By the same token, knowing about a society’s health and medicine helps us to understand important aspects of its culture.

An interesting example of culture in this regard is seen in Japan’s aversion to organ transplants, which are much less common in that nation than in other wealthy nations. Japanese families dislike disfiguring the bodies of the dead, even for autopsies, which are also much less common in Japan than other nations. This cultural view often prompts them to refuse permission for organ transplants when a family member dies, and it leads many Japanese to refuse to designate themselves as potential organ donors (Sehata & Kimura, 2009; Shinzo, 2004).Sehata, G., & Kimura, T. (2009, February 28). A decade on, organ transplant law falls short. The Daily Yomiuri [Tokyo], p. 3; Shinzo, K. (2004). Organ transplants and brain-dead donors: A Japanese doctor’s perspective. Mortality, 9(1), 13–26.
A society’s culture matters in these various ways, but so does its social structure, in particular its level of economic development and extent of government involvement in health-care delivery. Poor societies have much worse health than richer societies. At the same time, richer societies have certain health risks and health problems, such as pollution and liver disease (brought on by high alcohol use), that poor societies avoid. The degree of government involvement in health-care delivery also matters: the United States lags behind many Western European nations in several health indicators, in part because the latter nations provide much more national health care than does the United States. Although illness is often a matter of bad luck or bad genes, the society we live in can nonetheless affect our chances of becoming and staying ill.
Sociological Perspectives on Health and Medicine
The major sociological perspectives on health and medicine all recognize these points but offer different ways of understanding health and medicine that fall into the functional, conflict, and symbolic interactionist approaches. Together they provide us with a more comprehensive understanding of health, medicine, and society than any one approach can do by itself (Cockerham, 2009).Cockerham, W. C. (2009). Medical sociology (11th ed.). Upper Saddle River, NJ: Prentice Hall. "Theory Snapshot" summarizes what they say.
Theory Snapshot
| Theoretical perspective | Major assumptions |
|---|---|
| Functionalism | Good health and effective medical care are essential for the smooth functioning of society. Patients must perform the “sick role” in order to be perceived as legitimately ill and to be exempt from their normal obligations. The physician-patient relationship is hierarchical: the physician provides instructions, and the patient needs to follow them. |
| Conflict theory | Social inequality characterizes the quality of health and the quality of health care. People from disadvantaged social backgrounds are more likely to become ill and to receive inadequate health care. Partly to increase their incomes, physicians have tried to control the practice of medicine and to define social problems as medical problems. |
| Symbolic interactionism | Health and illness are social constructions: Physical and mental conditions have little or no objective reality but instead are considered healthy or ill conditions only if they are defined as such by a society. Physicians “manage the situation” to display their authority and medical knowledge. |
U.S. Health Care and the Industrial World
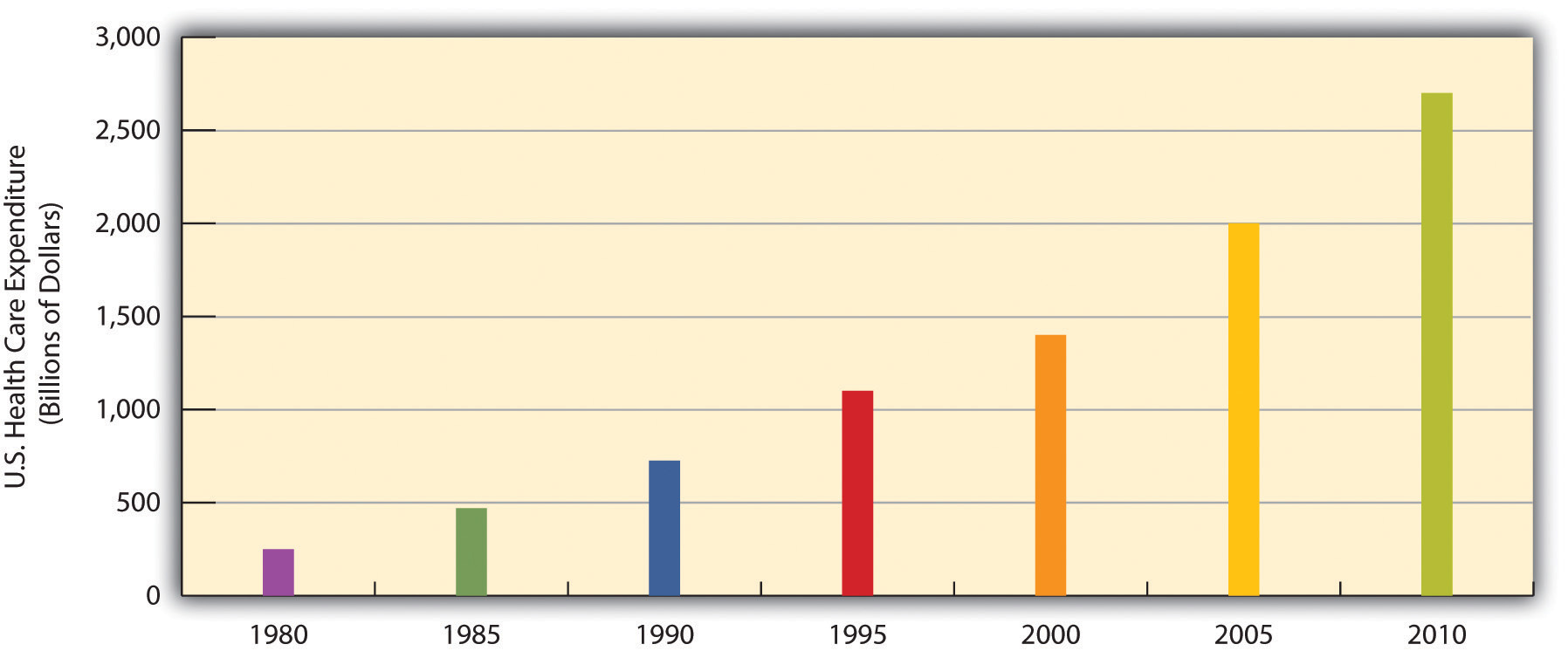
Medicine in the United States is big business. Expenditures for health care, health research, and other health items and services have risen sharply in recent years, having increased tenfold since 1980, and now costs the nation more than $2.6 trillion annually (see "U.S. Health-Care Expenditure, 1980–2010 (in Billions of Dollars)"). This translates to the largest figure per capita in the industrial world. Despite this expenditure, the United States lags behind many other industrial nations in several important health indicators, as we have already seen. Why is this so?
The U.S. Health-Care Model
Other Western nations have national systems of health care and health insurance. In stark contrast to these nations, the United States relies on a direct-fee system, in which patients are expected to pay for medical costs themselves, aided by private health insurance, usually through one’s employer. Figure 11.2.3 "Health Insurance Coverage in the United States, 2008" shows the percentages of Americans who have health insurance from different sources or who are not insured at all. (All figures are from the period before the major health-care reform package was passed by the federal government in early 2010.) Adding together the top two figures in the table, 57% of Americans have private insurance, either through their employers or from their own resources. Almost 28% have some form of public insurance (Medicaid, Medicare, other public), and 15.4% are uninsured. This final percentage amounts to about 46 million Americans, including 8 million children, who lack health insurance. Their lack of health insurance has deadly consequences because they are less likely to receive preventive health care and care for various conditions and illnesses. It is estimated that 45,000 people die each year because they do not have health insurance (Wilper et al., 2009).Wilper, A. P., Woolhandler, S., Lasser, K. E., McCormick, D., Bor, D. H., & Himmelstein, D. U. (2009). Health insurance and mortality in US adults. American Journal of Public Health, 99(12), 1–7.
| Employer | 52.3% |
| Individual | 4.7% |
| Medicaid | 14.1% |
| Medicare | 12.4% |
| Other public | 1.2% |
| Uninsured | 15.4% |
Although almost 28% of Americans do have public insurance, this percentage and the coverage provided by this insurance do not begin to match the coverage enjoyed by the rest of the industrial world. Although Medicare pays some medical costs for the elderly, we saw in that its coverage is hardly adequate, as many people must pay hundreds or even thousands of dollars in premiums, deductibles, coinsurance, and copayments. The other government program, Medicaid, pays some health-care costs for the poor, but many low-income families are not poor enough to receive Medicaid. Eligibility standards for Medicaid vary from one state to another, and a family poor enough in one state to receive Medicaid might not be considered poor enough in another state. The State Children’s Health Insurance Program (SCHIP), begun in 1997 for children from low-income families, has helped somewhat, but it, too, fails to cover many low-income children. Largely for these reasons, about two-thirds of uninsured Americans come from low-income families.
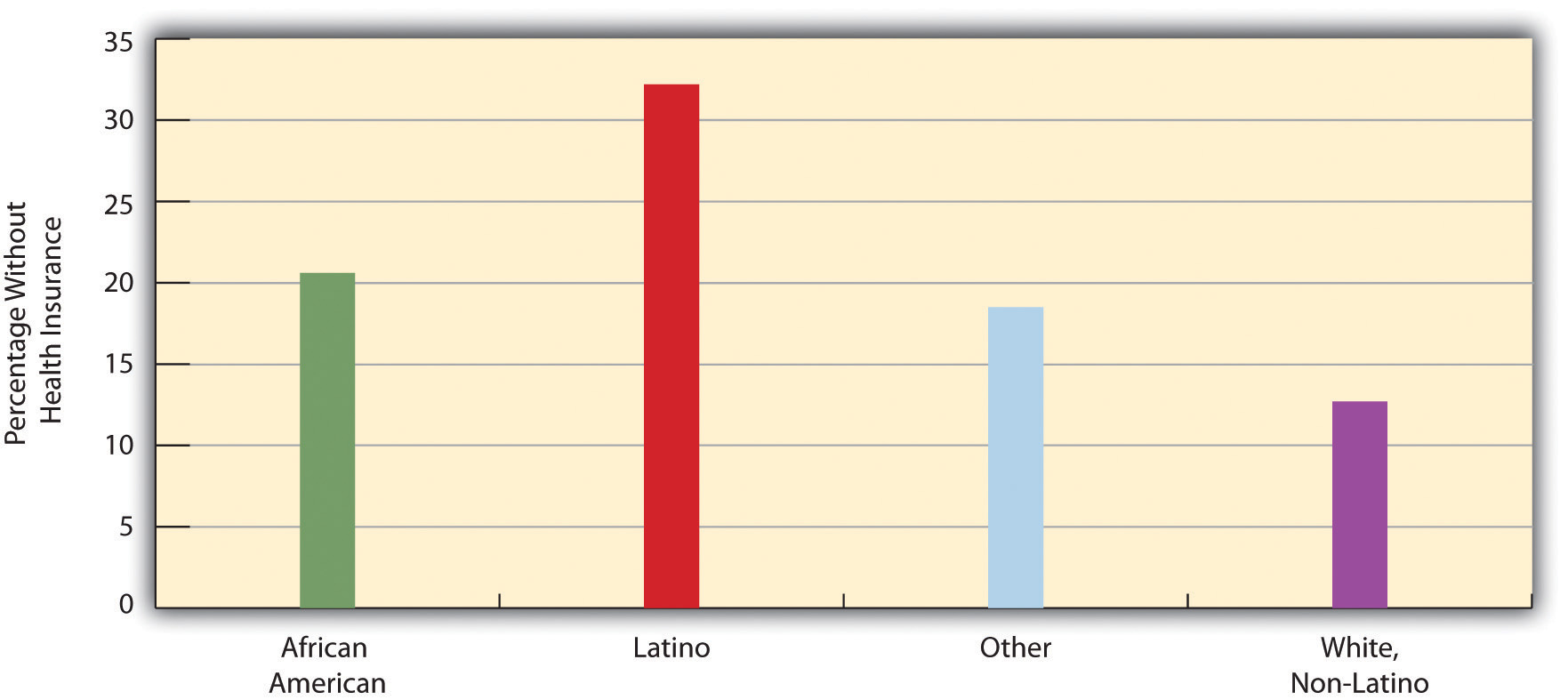
Not surprisingly, the 15.4% uninsured rate varies by race and ethnicity (see Figure 11.2.4 "Race, Ethnicity, and Lack of Health Insurance, 2008 (Percentage With No Insurance)"). Among people under 65 and thus not eligible for Medicare, the uninsured rate rises to almost 21% of the African American population and 32% of the Latino population. Moreover, 45.3% of adults under 65 who live in official poverty lack health insurance, compared to only about 6% of high-income adults (those with incomes higher than 4 times the poverty level). Almost one-fifth of poor children have no health insurance, compared to only 3.5% of children in higher-income families (Kaiser Family Foundation, 2010).Kaiser Family Foundation. (2010). Kaiser state health facts. Retrieved from http://www.statehealthfacts.org As discussed earlier, the lack of health insurance among the poor and people of color is a significant reason for their poorer health.
Issues in U.S. Health Care
The lack of insurance of so many Americans is an important health-care issue, but other issues about health care also seem to make the news almost every day. We examine a few of these here.
Managed Care and HMOs
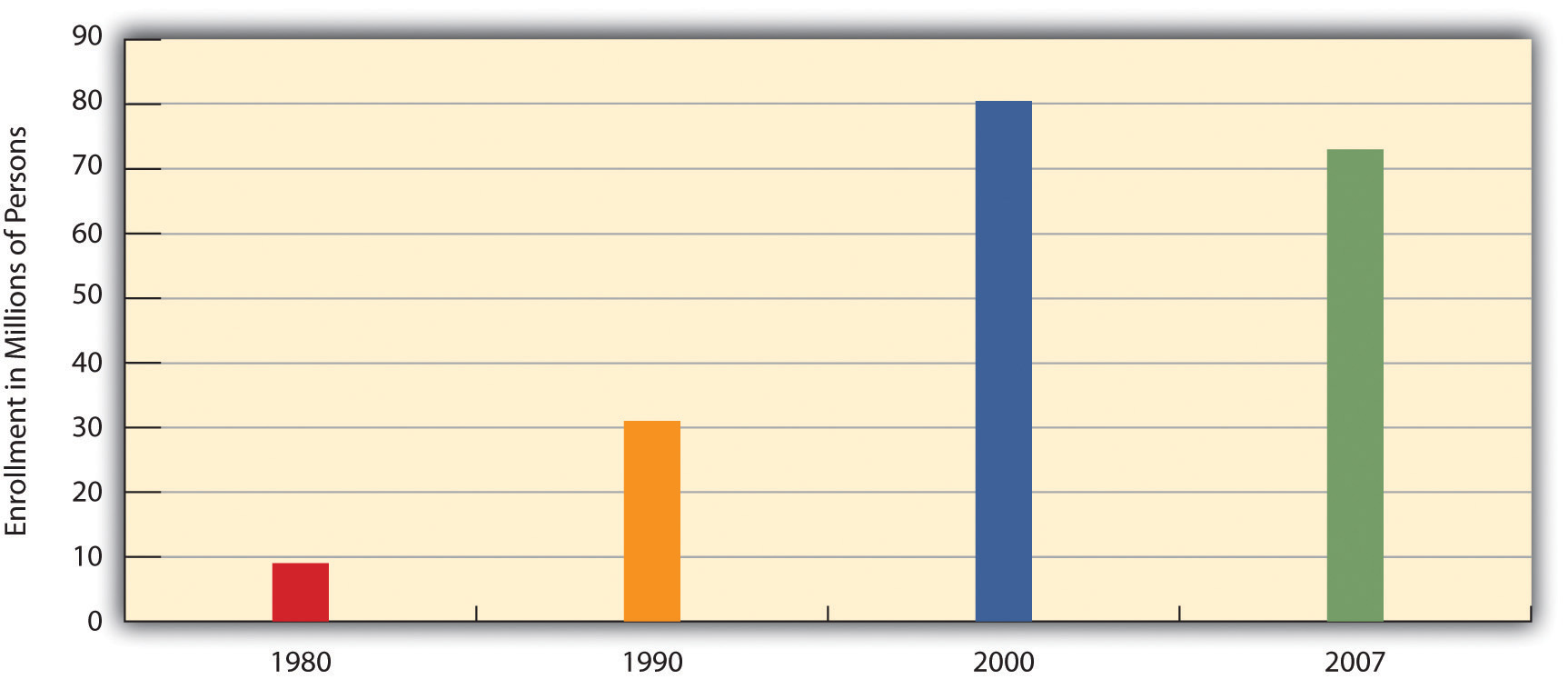
To many critics, a disturbing development in the U.S. health-care system has been the establishment ofhealth maintenance organizations, or HMOs, which typically enroll their subscribers through their workplaces. HMOs are prepaid health plans with designated providers, meaning that patients must visit a physician employed by the HMO or included on the HMO’s approved list of physicians. If their physician is not approved by the HMO, they either have to see an approved physician or see their own without insurance coverage. Popular with employers because they are less expensive than traditional private insurance, HMOs have grown rapidly in the last three decades and now enroll more than 70 million Americans (see Figure 11.2.5 "Growth of Health Maintenance Organizations (HMOs), 1980–2007 (Millions of Enrollees)").
Although HMOs have become popular, their managed care is also very controversial for at least two reasons (Kronick, 2009).Kronick, R. (2009). Medicare and HMOs—the search for accountability. New England Journal of Medicine, pp. 2048–2050.
Retrieved from www.library.umaine.edu/auth/EZProxy/test/authej.asp?url=http://search.ebscohost.com/login.as...=ehost-liveThe first is the HMOs’ restrictions just noted on the choice of physicians and other health-care providers. Families who have long seen a family physician but whose employer now enrolls them in an HMO sometimes find they have to see another physician or risk going without coverage. In some HMOs, patients have no guarantee that they can see the same physician at every visit. Instead, they see whichever physician is assigned to them at each visit. Critics of HMOs argue that this practice prevents physicians and patients from getting to know each other, reduces patients’ trust in their physician, and may for these reasons impair patient health.
The second reason for the managed-care controversy is perhaps more important. HMOs often restrict the types of medical exams and procedures patients may undergo, a problem called denial of care, and limit their choice of prescription drugs to those approved by the HMO, even if their physicians think that another, typically more expensive drug would be more effective. HMOs claim that these restrictions are necessary to keep medical costs down and do not harm patients.
Several examples of the impact of managed care’s denials of coverage and/or care exist. In one case, a woman with a bone spur on her hip had successful arthroscopic surgery instead of open hip surgery, the more common and far more expensive procedure for this condition. When her insurance company denied coverage for her arthroscopic surgery, the patient had to pay doctor and hospital fees of more than $21,000. After a lengthy appeal process, the insurance company finally agreed to pay for her procedure (Konrad, 2010).Konrad, W. (2010, February 5). Fighting denied claims requires perseverance. The New York Times, p. B6. In a more serious case a decade ago, a 22-year-old woman died after going to a physician several times in the preceding week with chest pain and shortness of breath. She was diagnosed with a respiratory infection and “panic attacks” but in fact had pneumonia and a blood clot in her left lung. Her physician wanted her to have lab tests that would have diagnosed these problems, but her HMO’s restrictions prevented her from getting the tests. A columnist who wrote about this case said that “an unconscionable obsession with the bottom line has resulted in widespread abuses in the managed-care industry. Simply stated, there is big money to be made by denying care” (Herbert, 1999, p. A25).Herbert, B. (1999, July 15). Money vs. reform. The New York Times, p. A25.
Inequality and Health
Health by Race and Ethnicity
When looking at the social epidemiology of the United States, it is hard to miss the disparities among races. The discrepancy between black and white Americans shows the gap clearly; IN 2008, the average life expectancy for white males was approximately five years longer than for black males: 75.9 compared to 70.9. An even stronger disparity was found in 2007: the infant mortality rate for blacks was nearly twice that of whites at 13.2 compared to 5.6 per 1,000 live births (U.S. Census Bureau 2011). According to a report from the Henry J. Kaiser Foundation (2007), African Americans also have higher incidence of several other diseases and causes of mortality, from cancer to heart disease to diabetes. In a similar vein, it is important to note that ethnic minorities, including Mexican Americans and Native Americans, also have higher rates of these diseases and causes of mortality than whites.
Lisa Berkman (2009) notes that this gap started to narrow during the Civil Rights movement in the 1960s, but it began widening again in the early 1980s. What accounts for these perpetual disparities in health among different ethnic groups? Much of the answer lies in the level of health care that these groups receive. The National Healthcare Disparities Report (2010) shows that even after adjusting for insurance differences, racial and ethnic minority groups receive poorer quality of care and less access to care than dominant groups. The Report identified these racial inequalities in care:
- Black Americans, American Indians, and Alaskan Natives received inferior care than Caucasian Americans for about 40 percent of measures
- Asian ethnicities received inferior care for about 20 percent of measures
- Among whites, Hispanic whites received 60 percent inferior care of measures compared to non-Hispanic whites (Agency for Health Research and Quality 2010). When considering access to care, the figures were comparable.
Health by Socio-Economic Status (SES)
Discussions of health by race and ethnicity often overlap with discussions of health by socioeconomic status, since the two concepts are intertwined in the United States. As the Agency for Health Research and Quality (2010) notes, “racial and ethnic minorities are more likely than non-Hispanic whites to be poor or near poor,” so many of the data pertaining to subordinate groups is also likely to be pertinent to low socioeconomic groups. Marilyn Winkleby and her research associates (1992) state that “one of the strongest and most consistent predictors of a person's morbidity and mortality experience is that person's socioeconomic status (SES). This finding persists across all diseases with few exceptions, continues throughout the entire lifespan, and extends across numerous risk factors for disease.”

A related reason for the poor health of poor people is unhealthy lifestyles, as just implied. Although it might sound like a stereotype, poor people are more likely to smoke, to eat high-fat food, to avoid exercise, to be overweight, and, more generally, not to do what they need to do (or to do what they should not be doing) to be healthy (Pampel, Krueger, & Denney, 2010; Cubbins & Buchanan, 2009).Pampel, F. C., Krueger, P. M., & Denney, J. T. (2010, June). Socioeconomic disparities in health behaviors. Annual Review of Sociology, 36, 349–370. doi:10.1146/annurev.soc.012809.102529; Cubbins, L. A., & Buchanan, T. (2009). Racial/ethnic disparities in health: The role of lifestyle, education, income, and wealth. Sociological Focus, 42(2), 172–191. Scholars continue to debate whether unhealthy lifestyles are more important in explaining poor people’s poor health than factors such as lack of access to health care, stress, and other negative aspects of the social and physical environments in which poor people live. Regardless of the proper mix of reasons, the fact remains that the poor have worse health.
It is important to remember that economics are only part of the SES picture; research suggests that education also plays an important role. Phelan and Link (2003) note that many behavior-influenced diseases like lung cancer (from smoking), coronary artery disease (from poor eating and exercise habits), and AIDS initially were widespread across SES groups. However, once information linking habits to disease was disseminated, these diseases decreased in high SES groups and increased in low SES groups. This illustrates the important role of education initiatives regarding a given disease, as well as possible inequalities in how those initiatives effectively reach different SES groups.
Health by Gender
Women are affected adversely both by unequal access to and institutionalized sexism in the health care industry. According a recent report from the Kaiser Family Foundation, women experienced a decline in their ability to see needed specialists between 2001 and 2008. In 2008, one quarter of females questioned the quality of her health care (Ranji and Salganico 2011). In this report, we also see the explanatory value of intersection theory. Feminist sociologist Patricia Hill Collins developed this theory, which suggests we cannot separate the effects of race, class, gender, sexual orientation, and other attributes. Further examination of the lack of confidence in the health care system by women, as identified in the Kaiser study, found, for example, women categorized as low income were more likely (32 percent compared to 23 percent) to express concerns about health care quality, illustrating the multiple layers of disadvantage caused by race and sex.

We can see an example of institutionalized sexism in the way that women are more likely than men to be diagnosed with certain kinds of mental disorders. Psychologist Dana Becker notes that 75 percent of all diagnoses of Borderline Personality Disorder (BPD) are for women according to the Diagnostic Statistical Manual of Mental Disorders. This diagnosis is characterized by instability of identity, of mood, and of behavior, and Becker argues that it has been used as a catch-all diagnosis for too many women. She further decries the pejorative connotation of the diagnosis, saying that it predisposes many people, both within and outside of the profession of psychotherapy, against women who have been so diagnosed (Becker).
Many critics also point to the medicalization of women’s issues as an example of institutionalized sexism. Medicalization refers to the process by which previously normal aspects of life are redefined as deviant and needing medical attention to remedy. Historically and contemporaneously, many aspects of women’s lives have been medicalized, including menstruation, pre-menstrual syndrome, pregnancy, childbirth, and menopause. The medicalization of pregnancy and childbirth has been particularly contentious in recent decades, with many women opting against the medical process and choosing a more natural childbirth. Fox and Worts (1999) find that all women experience pain and anxiety during the birth process, but that social support relieves both as effectively as medical support. In other words, medical interventions are no more effective than social ones at helping with the difficulties of pain and childbirth. Fox and Worts further found that women with supportive partners ended up with less medical intervention and fewer cases of postpartum depression. Of course, access to quality birth care outside of the standard medical models may not be readily available to women of all social classes.
Other Problems in the Quality of Care
Other problems in the quality of medical care also put patients unnecessarily at risk. These include:
Sleep Deprivation Among Health-Care Professionals
As you might know, many physicians get very little sleep. Studies have found that the performance of surgeons and medical residents who go without sleep is seriously impaired (Institute of Medicine, 2008).Institute of Medicine. (2008). Resident duty hours: Enhancing sleep, supervision, and safety. Washington, DC: National Academies Press. One study found that surgeons who go without sleep for 24 hours have their performance impaired as much as a drunk driver. Surgeons who stayed awake all night made 20% more errors in simulated surgery than those who slept normally and took 14% longer to complete the surgery (Wen, 1998).Wen, P. (1998, February 9). Tired surgeons perform as if drunk, study says. The Boston Globe, p. A9
Shortage of Physicians and Nurses
Another problem is a shortage of physicians and nurses (Shirey, McDaniel, Ebright, Fisher, & Doebbeling, 2010; Fuhrmans, 2009).Shirey, M. R., McDaniel, A. M., Ebright, P. R., Fisher, M. L., & Doebbeling, B. N. (2010). Understanding nurse manager stress and work complexity: Factors that make a difference. The Journal of Nursing Administration, 40(2), 82–91; Fuhrmans, V. (2009, January 13). Surgeon shortage pushes hospitals to hire temps. The Wall Street Journal, p. A1. This is a general problem around the country, but even more of a problem for two different settings. The first such setting is hospital emergency rooms, Because emergency room work is difficult and relatively low-paying, many specialist physicians do not volunteer for it. Many emergency rooms thus lack an adequate number of specialists, resulting in potentially inadequate emergency care for many patients.
Rural areas are the second setting in which a shortage of physicians and nurses is a severe problem. The National Rural Health Association (2010)National Rural Health Association. (2010). What’s different about rural health care? Retrieved from http://www.ruralhealthweb.org/go/left/about-rural-health points out that although one-fourth of the U.S. population is rural, only one-tenth of physicians practice in rural areas. Compounding this shortage is the long distances that patients and emergency medical vehicles must travel and the general lack of high-quality care and equipment at small rural hospitals. Partly for these reasons, rural residents are more at risk than urban residents for health problems, including mortality. For example, only one-third of all motor vehicle accidents happen in rural areas, but two-thirds of all deaths from such accidents occur in rural areas. Rural areas are also much more likely than urban areas to lack mental health services.
Mistakes by Hospitals
Partly because of sleep deprivation and the shortage of health-care professionals, hundreds of thousands of hospital patients each year suffer from mistakes made by hospital personnel. They receive the wrong diagnosis, are given the wrong drug, have a procedure done on them that was really intended for someone else, or incur a bacterial infection. These and other mistakes are thought to kill almost 200,000 patients per year, or almost 2 million every decade (Crowley & Nalder, 2009).Crowley, C. F., & Nalder, E. (2009, August 9). Secrecy shields medical mishaps from public view. San Francisco Chronicle, p. A1.
Complementary and Alternative Medicine (CAM)
As the medical establishment grew in the 19th and 20th centuries, it helped formulate many standards for medical care and training, including licensing restrictions that prevent anyone without a degree from a recognized medical school from practicing medicine. As noted earlier, some of its effort stemmed from well-intentioned beliefs in the soundness of a scientific approach to medical care, but some of it also stemmed from physicians’ desire to “corner the market” on health care, and thus raise their profits, by keeping other health practitioners such as midwives out of the market.
There is increased recognition today that physical health depends at least partly on psychological well-being. As the old saying goes, your mind can play tricks on you, and a growing amount of evidence suggests the importance of a sound mind for a sound body. Many studies have found that stress reduction can improve many kinds of physical conditions and that high levels of stress can contribute to health problems (B. W. Smith et al., 2010).Smith, B. W., Papp, Z. Z., Tooley, E. M., Montague, E. Q., Robinson, A. E., & Cosper, C. J. (2010). Traumatic events, perceived stress and health in women with fibromyalgia and healthy controls. Stress & Health: Journal of the International Society for the Investigation of Stress, 26(1), 83–93.

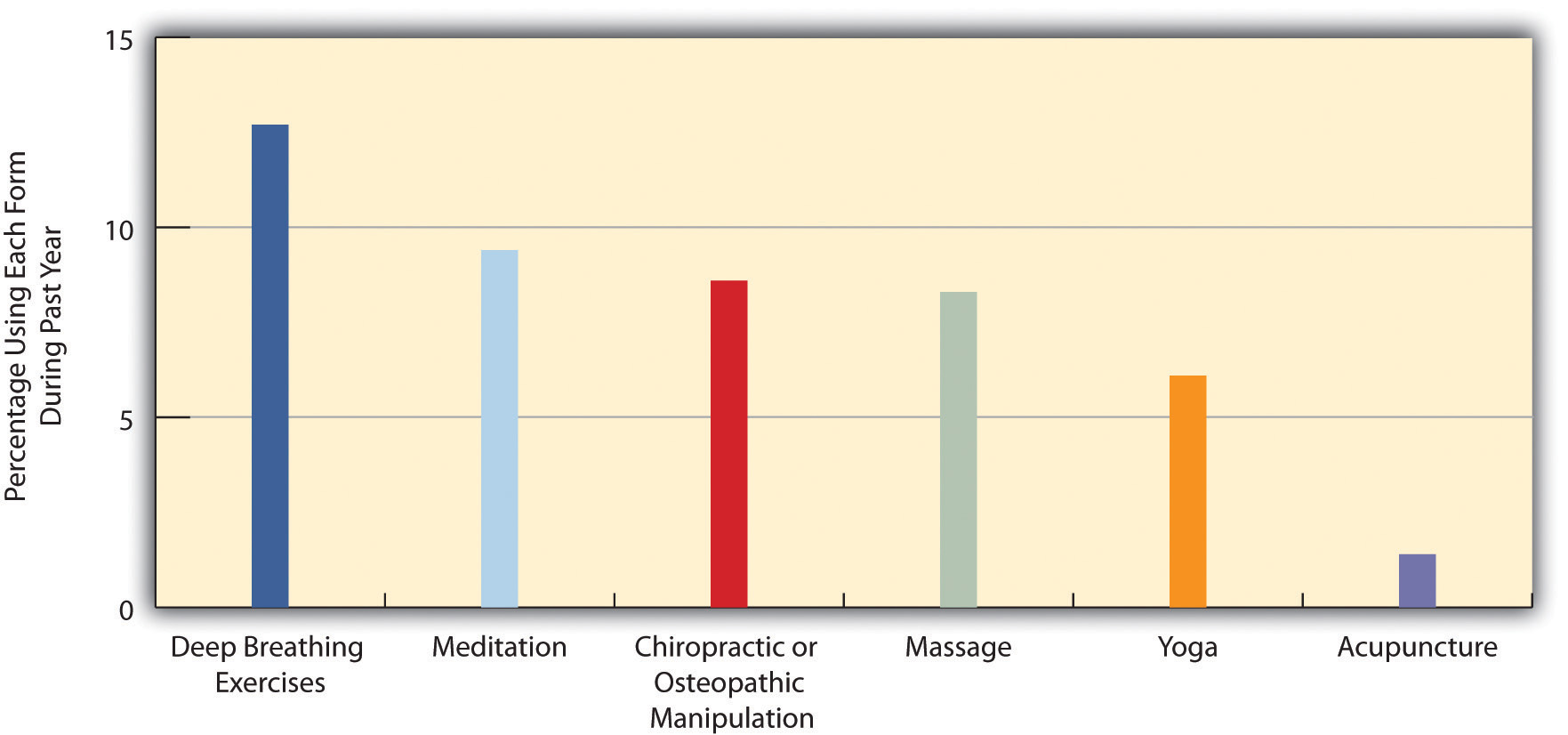
Evidence of a mind-body connection has fueled the growing interest in complementary and alternative medicine (CAM) that takes into account a person’s emotional health and can often involve alternative treatments such as acupuncture and hypnosis. In the last two decades, several major medical centers at the nation’s top universities established alternative medicine clinics. Despite the growing popularity of alternative medicine, much of the medical establishment remains skeptical of its effectiveness. Even so, about 40% of Americans use an alternative medicine product or service each year, and they spend about $34 billion per year on the various kinds of products and services that constitute alternative medicine (Wilson, 2009)Wilson, P. (2009). Americans spend $33.9 billion a year on alternative medicine.Consumer Reports Health Blog.
Retrieved from blogs.consumerreports.org/health/2009/08/information-on-natural-medicine-money-spent-on-alternative- medicine-alternative-treatments-vitamins.html